In what has been described as one of the most intellectually charged and emotionally stirring health conversations of the year, the National Association of Resident Doctors (NARD) in collaboration with the Resourceful Youth Network Initiative (RYNI) held the National Healthcare Summit 2025 virtually on Saturday, July 12, bringing together some of the most influential voices in Nigerian medicine—both at home and in the diaspora.
With the compelling theme “The JAPA Syndrome – Brain Gain or Brain Drain? Navigating the Future of the Nigerian Healthcare Sector,” the summit recorded massive participation from doctors across Nigeria and around the globe via Zoom. The virtual summit featured high-level stakeholders, including doctors from across Nigeria, the UK, US, and the Middle East, as they dissected the realities, root causes, and possible solutions to the mass migration of Nigerian doctors.
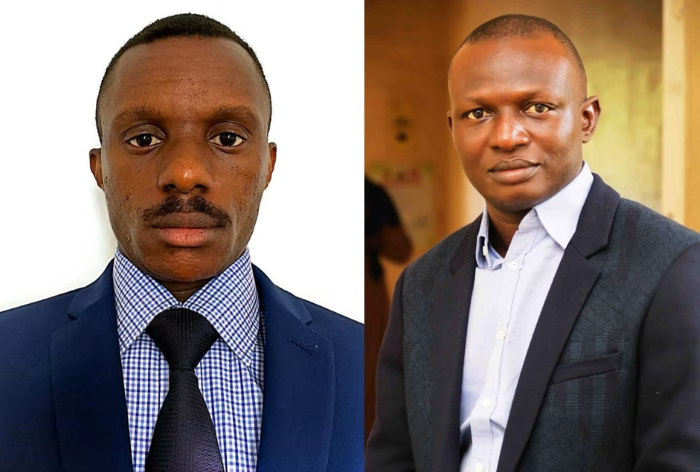
The event kicked off with strong opening remarks by the host as well as moderator, Dr. Osundara Tope, President of NARD, and the co-host and moderator, Dr. Lawson Obazenu, CEO of RYNI and a UK-based physician. Dr. Osundara called the Japa trend a “national emergency,” urging strategic engagement between government, local professionals, and diaspora doctors to halt the drain. Dr. Obazenu emphasized that the conversation should move beyond blame to building bridges that convert the brain drain into brain gain.
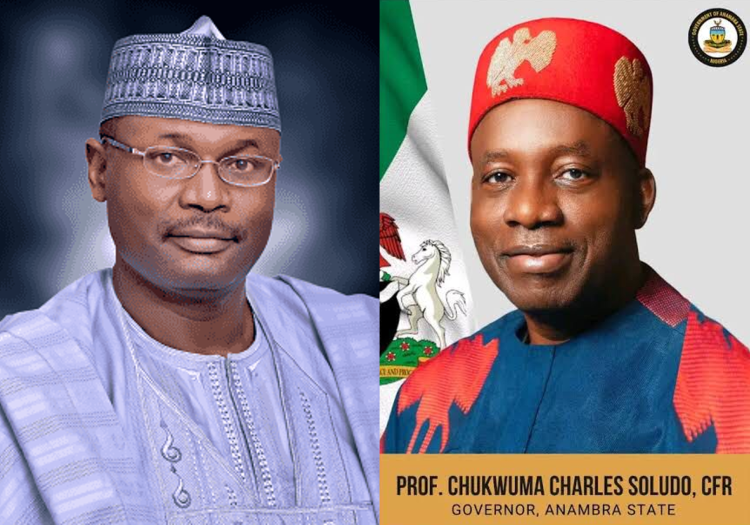
Delivering the keynote, Dr. Jimoh Salaudeen (mni), Director of Hospital Services, Federal Ministry of Health, acknowledged the troubling outflow of Nigerian doctors and admitted that diaspora doctors remain underutilized. He pledged stronger partnerships between the Federal Ministry of Health and diaspora organizations to institutionalize avenues for brain gain, including collaborative missions, specialist training, and technology transfer. “We must stop seeing diaspora doctors as gone. They are an untapped national resource,” he noted.
Prof. Bala Audu, President of the Nigerian Medical Association (NMA), warned of a bleak future if urgent reforms are not initiated. “We are not just losing doctors, we’re losing mentors, specialists, and future trainers. The system is collapsing from the inside,” he lamented. He further criticized medical tourism as a national contradiction and called for investment in local systems.
He also condemned the government’s move to export doctors to Saint Lucia, calling it “morally unjustifiable” in a country already crippled by severe doctor shortages.
Representing the UK diaspora, Dr. Elizabeth Fajemirokun, a Consultant Anaesthetist, advocated for inclusive reform led by doctors—not civil servants. She recommended rotational postings in high-performing private hospitals to improve resident training and morale.
In a poignant reflection, Dr. Solomon Oke, President of the Nigerian Doctors in UK (NDUK), admitted that his departure from Nigeria was not solely economic. “It was about safety, career structure, and hope. Nigeria didn’t offer that,” he said. He advocated for digital platforms that allow diaspora doctors to contribute remotely.
Similarly, Dr. Babagana Abubakar, a Saudi-based surgeon, emphasized that individual contributions by diaspora doctors are difficult due to systemic obstacles. He called for formal government-diaspora partnerships, medical missions, and specialist exchange programs to enable structured contributions.
In his final words, Dr. Lawson Obazenu, RYNI CEO, affirmed: “The narrative has changed. From JAPA to return, from brain drain to brain gain—this is our movement. Let us light the fire of transformation, and let it burn across every hospital, every state, and every diaspora corner of the globe.”
Consequently, panelists at the summit unanimously agreed that the Japa trend is not inherently evil, but its current trajectory is dangerous without a national strategy. They advocated Structural reform of training programs and healthcare financing, Leveraging diaspora doctors through partnerships and better wages, safer working environments, and clear career progression pathways.